Understanding Diabetic Eye Diseases; Risk & Prevention
Living with diabetes means keeping a close eye on more than your blood sugar — it means protecting your vision, too. We believe it’s important for our patients to understand how diabetes affects eye health and what steps can be taken to prevent vision loss.
How Diabetes Affects the Eyes
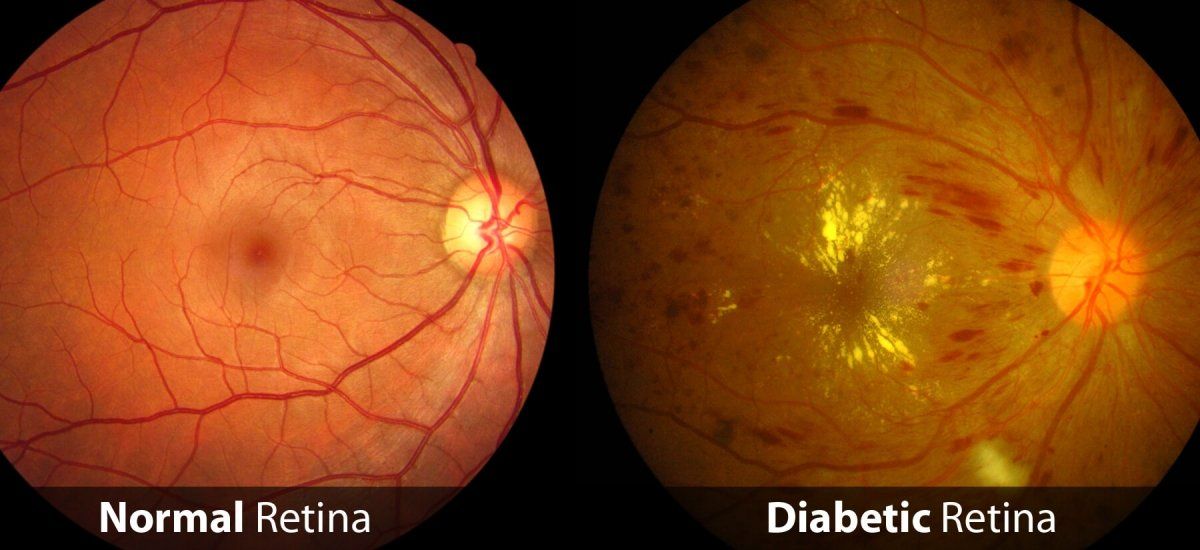
When blood sugar levels stay elevated over time, they can damage the tiny blood vessels in the retina — the light-sensitive tissue at the back of the eye. This damage can lead to a group of conditions known as diabetic eye disease, which includes:
1. Diabetic Retinopathy
The most common form of diabetic eye disease, retinopathy occurs when weakened blood vessels swell, leak fluid or blood into the retina or close completely. This results in bleeding/hemorrhaging in the retina as well as small outpouching of blood vessels, called microaneurysms. In advanced stages, abnormal new blood vessels may grow, increasing the risk of bleeding and scarring that can permanently affect vision.
2. Diabetic Macular Edema (DME)
When fluid leaks into the macula (the central area of the retina responsible for sharp vision), it causes swelling and blurry vision. DME is a leading cause of vision loss in people with diabetic retinopathy.
3. Ischemia and Neovascularization
Patients with diabetic retinopathy can develop poor blood flow in the retina, called ischemia, which can lead to poor vision. This can often cause new blood vessels to develop, which is called neovascularization. Retinal neovascularization can result in large bleeds in the eye and create retinal detachments. Both of these issues can result in significant loss of vision.
4. Cataracts
People with diabetes and uncontrolled blood sugars are more likely to develop cataracts — clouding of the eye’s natural lens — and often at a younger age.
5. Glaucoma
Diabetes can also double the risk of glaucoma, a condition that damages the optic nerve, often without early warning signs which can lead to permanent vision loss. Diabetes can also be a risk factor for other eye diseases such as a central retinal vein occlusion (CRVO).
Warning Signs to Watch For
Diabetic eye disease often develops silently, without noticeable symptoms at first. As the condition progresses, you may experience:
- Blurry or fluctuating vision
- Dark or missing areas in your sight
- Colors that appear faded or washed out
- Sudden vision loss in one eye
If you experience any of these changes, it’s important to schedule an eye exam right away.
Prevention and Protection
Most diabetes-related vision loss is preventable with early detection and proper management. Protect your vision by following these key steps:
- Get a yearly dilated eye exam. Early detection is the best defense against vision loss.
- Keep blood sugar, blood pressure, and cholesterol under control. Consistent management slows or prevents diabetic eye disease.
- Don’t ignore vision changes. Report even minor vision fluctuations promptly.
- Adopt healthy habits. Eat a balanced diet, exercise regularly, and avoid smoking — all of which support long-term eye health.
The Role of Regular Eye Exams
A comprehensive, dilated eye exam allows your doctor to see inside the eye and detect diabetic changes before they cause symptoms. Early treatment — whether through laser treatments or injections of medication in to the eye — can often help to reverse the damage done by diabetic retinopathy, and therefore, preserve and protect your vision.
Take Charge of Your Eye Health
At Talley Eye Institute, our experienced retina team provides specialized care for patients with diabetes. We work closely with your primary care physician, optometrist or endocrinologist to monitor your eye health and catch changes early.